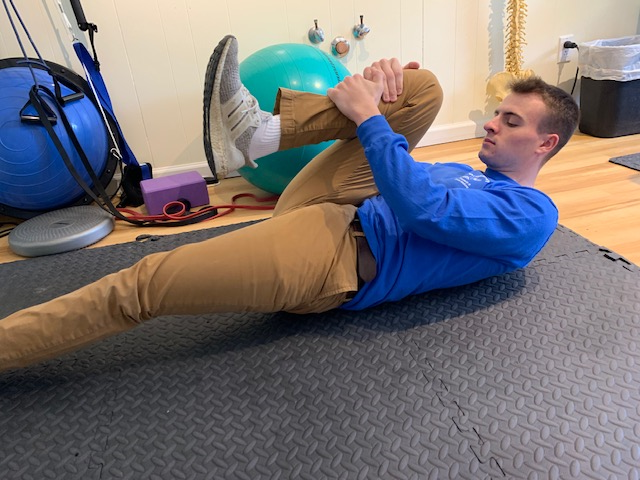
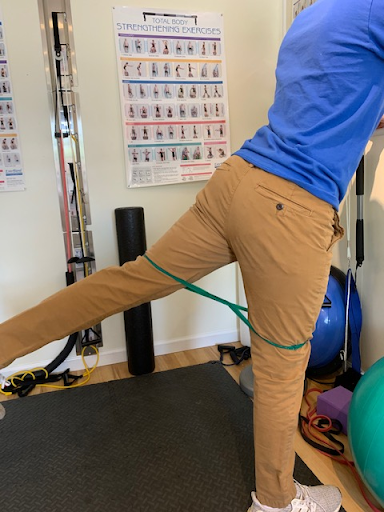
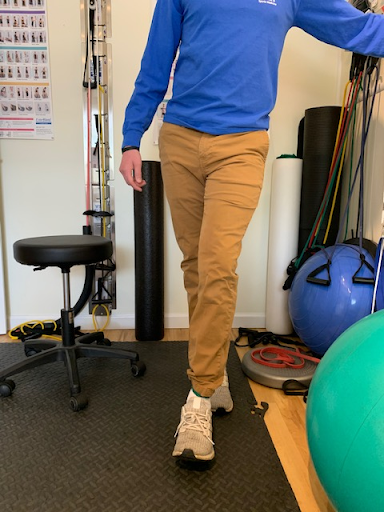
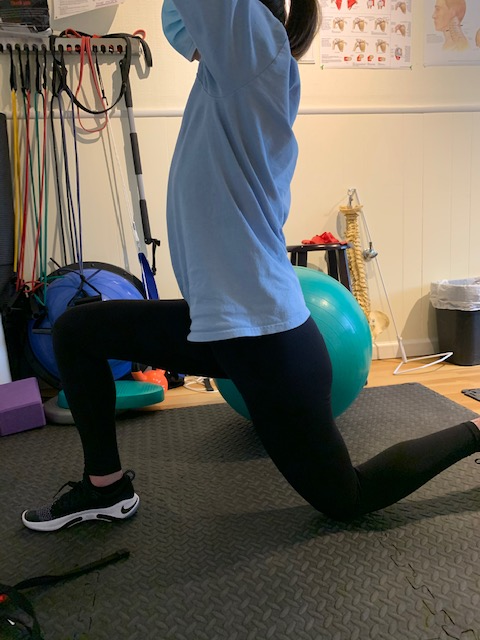
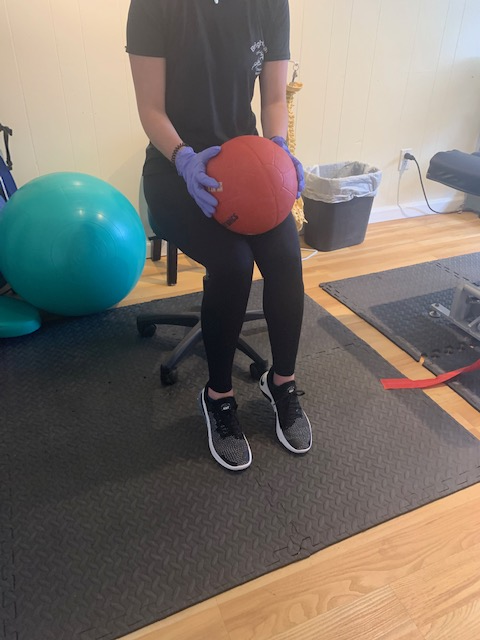
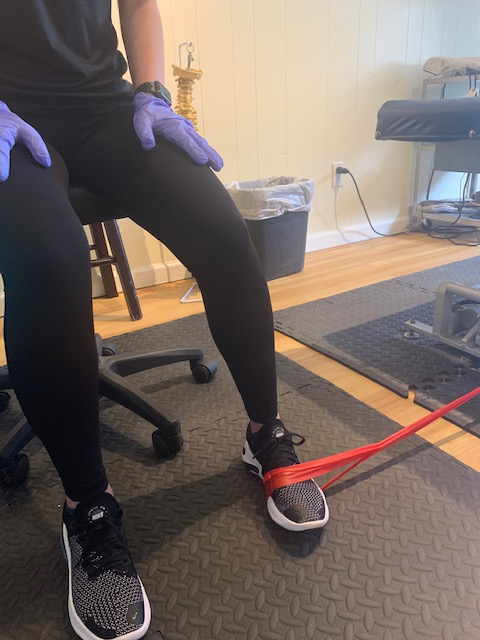
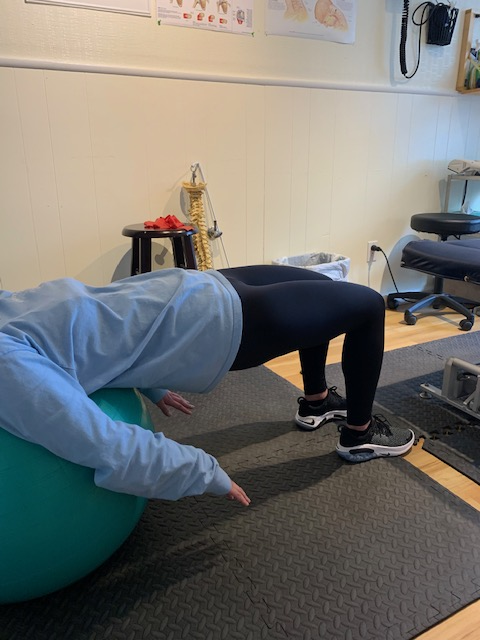
Conservative care for hip pain; Management with chiropractic care and therapeutic exercise5/22/2020 William Brightman DC, MS, MEd Hip pain has become very common in this day and age. I see it in my office on a daily basis and it is not just the older population. From school age through adulthood, people are afflicted with hip pain. The causes of hip pain are vast and varied, but with many other musculoskeletal conditions, lifestyle influences the outcome. The hip joint is a basic ball and socket joint that is able to move in several planes of motion. The most common is flexion and extension- as what you would see with walking, sitting, climbing stairs, and exercises such as squats. When hips are in a flexed position for an extended period of time the hip flexor muscles shorten up. This shortening of hip flexors will cause stiffness- especially when trying to stand up- and eventually pain in the hips and possibly the low back. Over time this shortening of the hip flexors will impinge on the joints themselves causing further restrictions and more pain. Joint pain is different from muscle pain but when one structure is injured the other is undoubtedly influenced. There are other causes of hip pain that can come from structures around the hip and even from the low back. It is important to examine all the structures and see which ones are restricted or contributing to the pain. An orthopedic and neurological exam combined with specific palpation and testing individual muscles and joints can determine the cause of the problem. Palpation is a tool that has been largely overlooked in modern medicine because of advanced diagnostic testing, but can be a very valuable skill for the practitioner if they have kept on top of it. Palpation essentially means to clinically examine each anatomical structure with your hands identifying specific patterns of local or referred pain. I find it very effective in my office and have been able to diagnose problems that are overlooked. Ninety-five percent of the time the diagnosis can be made after the physical exam. However, sometimes it is necessary to take x rays to rule out any degenerative changes in the hip. Osteoarthritis of the hips leading to potential hip replacements is not uncommon and this surgery is not just happening to the elderly, but people who are considerably younger and in good overall health. Fortunately, the surgery is very successful if you are in need, but the goal is to avoid and prevent the hips from getting to the point of “bone on bone”. Some differential diagnoses of hip pain include the following: trochanteric bursitis; Iliotibial band (IT) syndrome; strain of hip abductors (muscles on the outside); hip adductors (muscles on the inside); hip extensors (muscles in the back of hip); hip joint restrictions; sacro-iliac syndrome; labral tears; osteoporosis and arthritis (osteo, rheumatoid, psoriatic). As a sports chiropractor I will manage the strains and joint restrictions and take care of any imbalances. The results with extremity and sacro-iliac manipulation are effective and when combined with a daily therapeutic stretch and a strengthening program, the results are very good. I will refer out to other specialists if I am suspicious of underlying problems. Blood work and advanced diagnostic imaging such as MRI’s or CT scans may be necessary. Collaboration with orthopedists and rheumatologists along with physical therapists is not uncommon in managing hip problems. If the patient has rheumatoid arthritis or osteoporosis, manipulation is contraindicated, and other techniques must be used to help manage symptoms. Another problem that I have seen in my office is hip impingement or femoral acetabular impingement syndrome (FAI). I have seen a high prevalence of this with power athletes. Athletes engaged in high velocity movements and speed are most at risk, but anyone can be afflicted. A soccer player who is sprinting and kicking a ball at a high rate of speed is an example of someone who may develop FAI. The hip joint gets so locked up they lose the ability to move it like a ball and socket joint. In fact, they tend to lose a high percentage of internal rotation. This is not a popular motion but critical to have in order to perform at a high level. Specific manipulation to the hip joint works very well to reduce symptoms and allow athletes to heal rapidly. In my opinion, manipulating the hip joint in several planes of motion combined with lengthening of the muscles is superior to any other approach at managing this syndrome. Manipulation to the hip region is effective at opening up joints and muscles that are restricted. (above left long axis manipulation and right soft tissue release) Shock wave therapy to help break up muscle restrictions around the hip (on left targeted pulse to gluteal muscles and on right to the Iliotibial band down the lateral thigh) Hip joint problems can be greatly managed through conservative care, awareness of posture (sitting for extended periods of time), and therapeutic exercises to keep joints mobile and muscles strong and long. Collaboration with other physicians is recommended if conservative care is not alleviating the symptoms. Sometimes, cortisone is needed to calm inflamed tissues, and surgery to repair or even replace a joint. Thankfully, most people can do better with some hands on care, minor changes to the program, and a little guidance along the way. Foam rollers and lacrosse balls can be used to release myofascial soft tissue restrictions. (The fascia is the covering or saran wrap on outside of muscle) Therapeutic exercises for the hip: Above shows different stretches for all the muscles that cross the hip joint. When performing a static stretch try and hold for at least 15 seconds for each pose. Two sets or to tolerance will go a long way in stretching the hip muscles. Strengthening exercise of the hip: Lateral glide to help stabilize the pelvis (hits the hip abductors) Hip flexion with therabands (note:bands are above knee: start on left and finish on right) Hip abduction (open chain exercise to strengthen gluteus medius→ helps to support hip and stabilize pelvis) Hip extension with therabands (open chain exercise to strengthen gluteus maximus which is powerful hip extension muscle) Hip rotation exercise: Internal rotation of the hip joint is one of the first motions to go and it is important to try and activate that motion Hip adduction: This will strengthen the hip adductors of the inner thigh Great hip and spine stabilizer! Hip extension combined with opposite shoulder in extension (The “bird-dog”- try without resistance then progress with body band) Glute bridge: great for hip extension and pelvic and low back stabilization Progressive bridge on physioball
William Brightman DC, MS, MEd Sports Chiropractor/Exercise Physiologist Private Practice, Mahopac, NY [email protected]
0 Comments
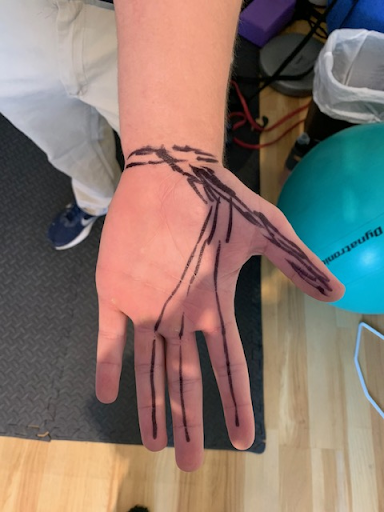
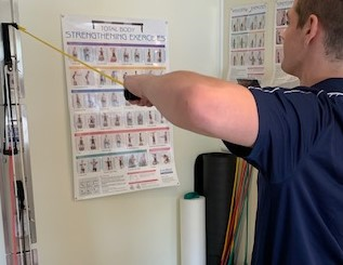
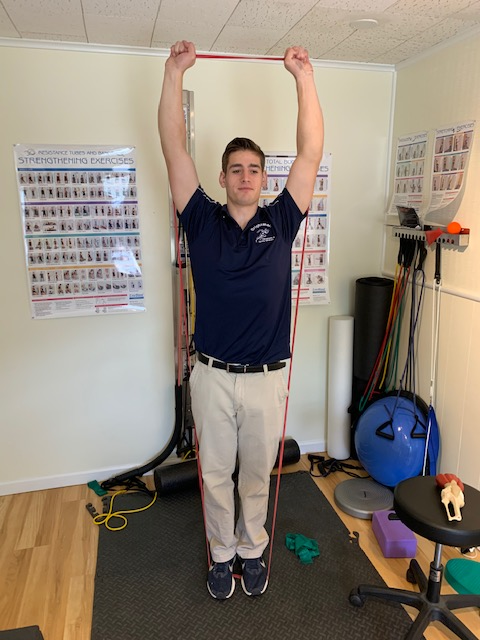
By William Brightman DC, MS, MEd At least several times a month I will have a patient present to the office complaining of “carpal tunnel”. We start off with a series of questions usually centered around “describe exactly what you're feeling”?, “point to where you feel it”?, “do you feel pain, tingling, burning, or numbness in the first three fingers”? ( technically ½ of the 4th -ring- finger). “ Is it worse at night”? “Are you dropping items”? “Do you have elbow, shoulder, or neck pain”? This is a basic history that any thorough practitioner should do to gain information. Next, I will do a series of provocative (almost annoying tests to reproduce the symptoms) tests that include orthopedic, neurological, and chiropractic assessments to isolate where the problem is. True carpal tunnel syndrome (CTS) is an entrapment of the median nerve as it traverses under a ligament in the wrist and slides through the carpal bones. The median nerve feeds the first three and one half digits controlling muscle movement and the skin that overlies it. The CTS patient will experience pain, numbness, and tingling in the first three and one-half fingers and there may be notable atrophy in the muscles of the thumb. Pain distribution of Carpal tunnel syndrome CTS affects 3-6% of the population and one of the primary causes is repetitive stress syndrome. Obesity, diabetes, pregnancy, arthritis, and hypothyroidism are all conditions that can increase the probability of developing CTS. Women tend to be at higher risk than men due in part to wrist size and influence of progesterone and estrogen. The diagnosis is made through the examination based on + findings. (which don’t feel so positive!). Sometimes, I will refer out to a neurologist to order an electromyographic nerve conduction velocity (EMG/NCV) exam to confirm my suspicions. The test is a diagnostic test that basically measures how fast the impulse is traveling down the arm to the hand and it will compare it to the other side. If the impulse slows down at the wrist then this could be indicative of CTS. At this point the sports chiropractor will treat and manage the CTS conservatively. It is important to note that there are several conditions that mimic CTS and they have to be diagnosed and treated for the patient to have success. Musculoskeletal problems from the elbow, shoulder, and neck may also mimic CTS and need to be evaluated. Non musculoskeletal problems that could refer to the hands could also be from the heart and lungs and should always be ruled out! The sports chiropractic approach to treating CTS overlaps with other standard approaches but is also uniquely different. For starters, night splint, anti inflammatory measures, therapeutic stretches, and ergonomic recommendations are made like most other practitioners. In addition, the sports chiropractor will adjust the carpal bones in the hand to help increase the diameter to where the median nerve travels through. (it will have more space). Finally, chiros will incorporate muscle release techniques in the forearm flexor muscles that help release some painful tissue. This combined with the traditional approach will yield superior results. Especially if symptoms are mild to moderate. If symptoms have persisted for an extensive period of time then surgery may be necessary. Manipulative techniques of upper extremity to release median nerve I have personally found this approach to be very good with the majority of patients. Some patients have eventually needed surgery and I have found that when it is necessary the results are also good with surgery. One study in 2018 demonstrated that extremity manipulation done by a highly skilled chiropractor to the hands increased the anterior to posterior diameter of the tunnel thereby decreasing symptoms related to CTS. Another 2019 study revealed that soft tissue techniques that addressed the muscles that crossed the tunnel concluded to be highly effective in a group of patients that suffered from mild to moderate CTS. I would personally agree with those studies. The key is to get a thorough exam with a diagnosis and treatment plan that makes sense. Start with conservative care such as PT and Chiropractic and if those treatments are falling short then seek a surgical opinion. Also, seek out a chiropractor trained in upper extremity manipulation. Sports Chiropractors have additional training in how to manage these conditions. Therapeutic exercises for Carpal tunnel syndrome: Therapeutic strengthening exercises of the forearm flexors Self stretch with release to forearm muscles that cross the wrist and tunnel
William Brightman DC, MS, MEd Sports Chiropractor/Exercise Physiologist Private Practice Mahopac NY Sports Medicine/ Anatomy & Physiology Instructor [email protected] By William Brightman DC, MS, MEd
Ever since I could remember I have always heard that exercise is “good for you”. But when you ask people what that means they find it hard to define. Some will say that it “makes you stronger”, or that it is “good for your heart”. Others get the mind body connection and will say that “it just makes me feel good” or “I do it for stress”. There is a whole field now built on the science of exercise- and there is a lot of science behind it! This article will shed a little light on some of that science in the hopes that some will participate in activity knowing a bit more detail. From my perspective, the “good for you” is not working with a large part of the population. Education is always important and may turn on the proverbial switch in the brain. People are motivated by different things and if something resonates in this article as to why you should start exercising then it is worth it. For starters, many avoid exercise because they think it has to be painful to get something out of it. This could not be further from the truth. In fact, most of the evidence supports consistent moderate physical activity is beneficial to not only obtaining better health but preventing disease. It is not necessary to exercise with high intensity unless you are an athlete competing at a high level. There are different types of exercise, and like nutrition, the term “exercise” can be confusing to the casual observer. For instance, nutrition is simple but it has been made complex with the myriad of diets that are out there. Likewise, exercise is simple but there are so many programs available that people get confused and are not sure what is best for them. The objective is to move and move often. This should vary from day to day and it should be a combination of physical activity and structured exercise. Physical activity can be as simple as walking, hiking, playing tennis, golf, skiing, dancing,volleyball, gardening, mowing the lawn, badminton- you name it- as long as the body is moving. Do what you enjoy doing and there will be some positive outcomes with physical activity only. However, to enjoy greater benefits of exercise it is important to have structured exercise at least three times a week for 30 minutes. This could include resistance training (anaerobic) with bodyweight exercises, exercise bands, machines, free weights or medicine balls. It could also include cardiovascular or aerobic type exercises such as brisk walking, jogging, cycling, swimming, or elliptical training. You could also set up a circuit of light weights and mover from station to station getting your heart rate up. There should probably be some form of flexibility for injury prevention as well. Athletes will also incorporate power, speed, agility, and balance to help with performance. These other forms of fitness are not just for athletes as anyone can incorporate them into their exercise routines. Mix it up, have fun with it and enjoy the benefits. Cardiovascular exercise is probably the most important of all the exercises because of its direct influence on the heart and cardiovascular system. 20-30 minutes of sustained aerobic exercise where the heart rate is elevated at 60-80% of your maximum heart rate will have profound effects on your overall health. (An estimated maximum heart rate is 220- age = maximum heart rate. A more accurate estimate of maximum heart rate is 206.9- (0.67 X age). The latter formula is recommended by the American College of Sports Medicine but is a little more complicated than the older formula. The differences are not that significant and either can be used to determine maximum heart rate. Then it’s a matter of multiplying by percentage to get a working heart rate. Plug in 60-80% and that will be your working heart rate. There are formula’s online to help you find your working heart rate. Cardiovascular exercise has so many benefits and the most important one is its impact on heart disease. Heart disease is our number one killer in society and aerobic exercise goes a long way in not only helping to prevent this disease, but is also useful in the management of the disease. How does aerobic exercise impact the cardiovascular system? For starters, it improves blood flow to the heart itself thereby feeding it. In fact, cardiovascular training may increase collateralization to the heart muscle. The coronary arteries of the heart may develop sideroads to feed the myocardial heart tissue. If there is a clog in one of the main arteries side streets can be used to go around the blockage. This is an amazing adaptation of the human body! The ability to lay down more vessels in order to feed the heart muscle. Consistent aerobic training can also strengthen the left ventricle thereby increasing the efficiency of how blood is pumped from the heart to the rest of the body. This in turn will lower one’s resting heart rate. Think about having a resting heart rate of 65 beats per minute versus 75 bpm. That’s 10 beats a minute, 600 beats an hour, 14,400 beats a day, 432,000 beats a month, and 5,184,000 beats a year! By training and growing your heart muscle (cardiac hypertrophy), your heart can save over 5 million beats throughout the year! Think how that can save your heart muscle over a lifetime. Resistive exercises have been shown to be beneficial to increasing muscle strength, endurance, and overall lean mass. There are thousands of studies showing that progressive resistive exercise such as weight training will increase muscle density and growth. Muscle density can also be beneficial as one ages in the prevention of sarcopenia. Sarcopenia is a gradual loss of muscle over time. This can contribute to weakness, loss of balance, frailty, and a decrease in quality of life. Resistive training can also help to increase bone density throughout your life. Progressive resistive weight training in your early years will help you in your later years. Loss of bone in early life will lead to osteopenia and eventually osteoporosis. Osteoporosis is a bone thinning disease. It has multiple causes but we do know that a lifestyle that includes resistive training can have a positive influence on bone density and prevent osteoporosis. While cardiovascular, muscle, and bone changes are most significant in the body with consistent exercise, there are many other benefits one can achieve with physical activity. These changes are more powerful than any medicine out there. In fact, if someone said that there is a pill that will help you with your heart, lungs, brain, nervous system, bones, muscles, and immune system would you take it? The answer is yes and it is right under your nose in the form of consistent exercise along with physical activity. Here are some other benefits with physical activity and structured exercise that you can expect with consistent training.
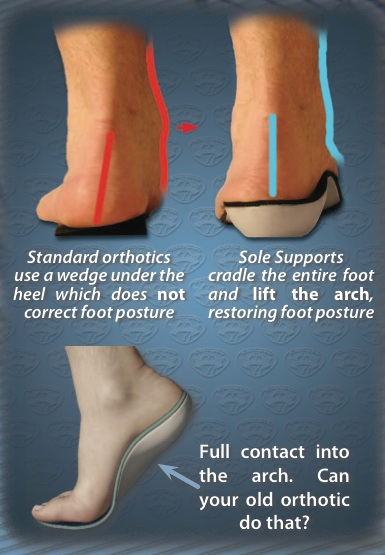
As you can see there are many benefits of physical activity along with structured exercise. I emphasize both throughout the article because there is a synergistic response when both are combined. You should not be a slave to exercise, but rather, enjoy getting out and moving most days of the week. If you accumulate 150 minutes a week of both then you are well on your way to the benefits of a lifetime! So yes, exercise is definately “good for you”! William Brightman DC, MS, MEd Sports Chiropractor Private practice Mahopac, NY [email protected] By William Brightman DC, MS, MEd “Runner’s knee” is a common term given to the type of athlete it impacts the most- runners. But people who develop runner’s knees are not always runners. It is a repetitive stress injury and can be brought on by any action done repeatedly over an extended period of time. Jumping, squatting, hiking, climbing stairs, and of course running are all causes of runner’s knee. There are other factors beyond the typical repetitive stress contributing to runner’s knee. This article will look at some of the other factors that contribute to runner’s knee and how it is managed conservatively with therapeutic exercise, physical therapy, and chiropractic care. The medical name for runner’s knee is patellofemoral syndrome. Symptoms of patellofemoral syndrome are pain around the knee that can be described as a dull throbbing ache that is caused from excessive activity but can be felt at rest or while exercising. Additional symptoms may be tenderness to the touch and clicking or popping of the tendons that cross the joint. When examined more closely the symptoms and diagnosis of “runner’s knee” goes beyond running. It is important to look at alignment, joint function, and muscle weaknesses in the lower extremity. Each of these may contribute to patellofemoral syndrome. The foot and hips are two regions that may influence the knee. Moreover, the muscles that cross the hips and knees have a direct impact on patellofemoral syndrome. Especially when they are weak or imbalanced. This is why it is critical to strengthen and bring these muscles into balance to correct the problem. Ice, anti-inflammatories, and rest are nice to alleviate symptoms but corrections require a program of guided treatment and therapeutic exercise in order to get more lasting results. Knee anatomy from the front and back Let’s start with the foot joint. The foot is amazingly complex and is composed of 26 bones and 33 joints. Misalignments in these bones can contribute to tracking problems of the knee. Overpronation of the foot has been closely associated with knee and hip problems as well as low back issues. Oftentimes, one “keystone” bone (navicular bone) may be falling further than the other bones and this may contribute to excessive overpronation- and instability to foot, ankle, and knee. This happens slowly and insidiously and the individual may not even know it is going on. When the “keystone” bone (navicular bone) falls the result is overpronation- this will contribute to runner’s knee. Adjustments to the bones of the feet combined with individual specific exercises and orthotics will help to correct the foot problem that is impacting the knee. Another structural problem that may contribute to runner’s knee is from the hips. Hip flexor muscles cross the hip joint and over time they can become shortened and contribute to hip and pelvic misalignments and joint restrictions. This in turn will shorten a major muscle called the rectus femoris which crosses both the hip and knee joint. When this muscle is shortened it will pull on the patella contributing to runners' knee. The treatment requires manipulation to the hip and pelvic (sacroiliac) joints and a program that stretches and strengthens the rectus femoris muscle. Muscles that cross the hips and knees may be imbalanced over time and should be addressed to bring up any weaknesses. Once weaknesses are addressed and strengthened then knee pain will often subside and heal. One treatment (i.e. ice & rest), is not sufficient in managing runner’s knee. It is easy to tell someone not to run but our job is to get them running safely, in the right shoes, and properly adjusted and strengthened. The knowledge the patient has is empowering! The individual with runner’s knee should make sure that they have proper running shoes (i.e. brooks or asics) and possibly orthotics (we recommend sole support orthotics) for further support to the arch. It is recommended to increase activities slowly, stretch before and after running and pay attention to good running mechanics (get video analysis and read articles on running biomechanics). If the runner is overweight, then a weight management program combined with brisk walking may be advised before running. These tips combined with corrective exercises and sports chiropractic care will yield fantastic results in the treatment and management of patellofemoral syndrome or runner’s knee. Below are some basic exercises that are helpful for Runner’s knee. Isolation exercises combined with stabilization exercises are best for condition. Terminal knee extension with foot rotated out and flexed to activate inner quadriceps. This muscle (vastus medialis) becomes weakened with repetitive stress and the patella tracks laterally- this exercise is a good place to start with a runner's knee. Hip abduction and flexion performed slowly to strengthen abductors and flexors Glute bridge for stabilization of pelvis Stretching the hip flexor (rectus femoris) Lateral band shuffle to activate gluteus medius(important to stabilize pelvis from side)
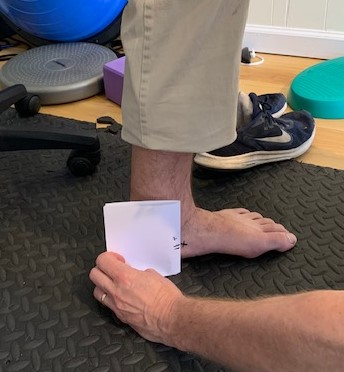
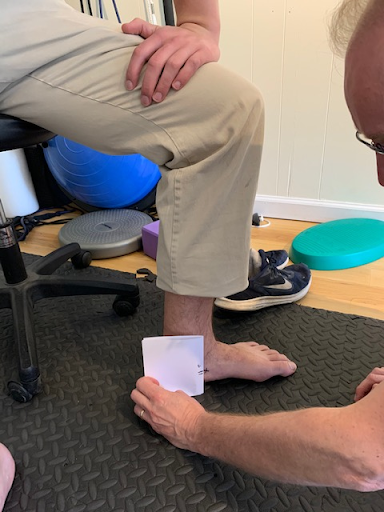
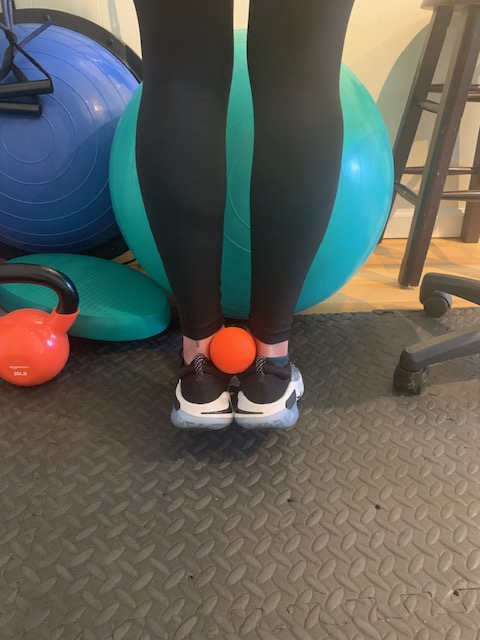
William Brightman DC, MS, MEd Sports Chiropractor Private Practice Mahopac, NY [email protected] How to effectively treat “shin splints” through sports chiropractic & therapeutic exercise5/20/2020 William Brightman DC, MS, MEd If you have ever suffered from “shin splints” you know it! Shin splints is the term given to a pain along the front or back part of the tibia bone in your lower leg. It is common among runners and dancers but does not discriminate against any athlete. In fact, any athlete who has increased their intensity, duration, or frequency in training- especially running- can become afflicted with this condition. Training on hard surfaces, uneven terrain, just beginning a running program, having high arches or fallen arches, military training, and even hiking can all be contributory factors in the prevalence of shin splints. “Shin splints” is also known as medial tibial stress syndrome and the symptoms associated with this condition are tenderness, soreness, and pain that increases with the activity but can also be painful at rest. With the early onset of shin splints, rest, ice and modified activities are recommended for treatment. That is all well and good but still does not solve the problem. In fact, the problem came on with training and goes away with rest, but who says that it will not come back again when training resumes. This is when a more focused evaluation needs to be done. The sports chiropractic evaluation is a more detailed assessment that looks at all the muscles and joints in the lower extremity to look for imbalances that may be contributing to the problem. The question arises as to why some athletes are more prone to “shin splints” than others? Like most other conditions there are many reasons as to why one athlete develops shin splints while another does not. Muscular imbalances, overpronation of the foot, or even hip and pelvic distortion can contribute to “shin splints' in one athlete while the more “muscularly balanced” athlete may avoid them. This will be assessed in a sports chiropractic exam. Two specific deep muscles in the lower extremity known as the tibialis anterior and tibialis posterior muscles are found to be vulnerable in shin splints. They are deep or “core” muscles in the calf and will become weak and imbalanced with repetitive stress and lack of attention. The consequence is “shin splints”. These muscles are tested for strength during the evaluation and more often than not are weak when the athlete has shin splints. Two most common areas where “shin splints” occur (tibialis anterior and tibialis posterior muscles become strained, weak, and imbalanced→ exercise on right help to address tibialis posterior muscle Feet that overpronate and arches that fall may be a trigger to shin splints as well as other problems in the lower extremity (In addition to therapeutic exercises and adjustments, orthotics may be necessary to make correction) Measurements can be done to see how far the arch is falling and can be compared to the arch of the other foot. Discrepancies that are clinically significant may warrant sole support orthotics The athlete who trains hard and is not paying attention to good running mechanics, does not have supportive footwear, and is not strengthening the deeper core muscles of the lower extremity may become susceptible to shin splints. If muscles become weak then the corresponding joints are impacted. For instance, the tibialis posterior muscle runs down to the bottom of the foot (tarsals) and when it becomes weakened or overstretched the tarsal joints restrict and the arch overpronates. This disruption in the tarsal (foot) joints will alter the mechanics during the run and one problem becomes overpronation of the foot. This overpronation will in turn contribute to an increased stress on the posterior tibia and eventually strain the muscle where it attaches to the tibia bone. This may cause a reaction to the bone and even a possible stress response fracture. Hence the term “shin splints”. Treatment usually starts with ice and rest. Physical therapy modalities such as ultrasound and muscle stimulation may be helpful to alleviate some of the symptoms. In our practice, I have found that adjusting the tarsal bones of the feet along with performing myofascial release to the deep calf muscles is incredibly effective at restoring motion and function in the lower kinetic chain (the foot and calf region) and reducing shin splint symptoms. Secondly, the athlete needs to be on a progressive strengthening program addressing all of the muscles of the lower extremity. There should be an emphasis on the superficial and deeper calf muscles. Finally, the athlete may need a video analysis to assess their overall running mechanics. Once imbalances are pointed out exercises can be provided. This evaluative and therapeutic approach, along with lower extremity, hip, and pelvic adjustments are most effective at healing and preventing future shin splints. The sports chiropractor takes this unique approach to treating shin splints. They will combine traditional methods (ice, modalities, anti inflammatories) with biomechanical evaluation (assessing joints and muscles) and treatments (muscle and joint manipulation with corrective exercise) that are highly effective. Below are some therapeutic exercises for shin splints. This combined with extremity and pelvic adjustments, myofascial release techniques, and appropriate footwear to support overpronation (sometimes orthotics are necessary) yields the best results! Seated calf raises for soleus medial foot glide for tibialis posterior muscle Standing calf raises while squeezing ball( develops larger gastrocnemius calf muscle while hitting deeper stability muscles: performing static stretch for 15-30 seconds after exercising muscle. Squats with theraband and hip hikes to help strengthen pelvic stabilizers. ( these exercises are good for most lower extremity problems including shin splints) Active Pin & Stretch to release tibialis anterior muscle (one of the culprits in shin splints)
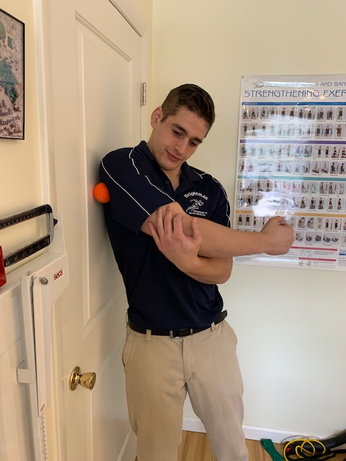
If you are experiencing “shin splints” consult your sports chiropractor for an evaluation and holistic approach to treatment. Several treatments combined with home instruction will correct the disorder. Diagnostic imaging (x rays, CT scan, or MRI) may be indicated if the problem has been persistent for a long period of time and has not responded to conservative treatment. Your sports chiropractor will only order these if it is absolutely necessary and the patient has not improved with care over 4-6 weeks. Standard protocol is to diagnose with examination, treat accordingly and re evaluate for progress. Results are usually superior to rest and anti-inflammatories alone. Try this multi disciplined holistic approach if you want to not only treat but prevent any future flare ups of shin splints. William Brightman DC, MS, MEd Sports Chiropractor/ Exercise Physiologist Private Practice Mahopac, NY [email protected] William Brightman DC, MS, MEd When I hear a patient say that their shoulder is in pain the first thing I ask them to do is point to where the pain is coming from. The patient may point to an area in the vicinity of the shoulder like the base of the neck (cervico-thoracic region), the collar bone and upper chest (clavicular-pectoral region), or the shoulder joint (glenohumeral) itself. They may also point to their shoulder blade close to the mid back (scapulo-thoracic region) to identify their source of pain. In other words, the term “shoulder” can cover a large region for most patients trying to describe their pain. Fortunately, most musculoskeletal pain can be identified with a complete hands on physical exam. Once the tissue(s) are identified and tested then a conservative approach can commence. The patient should start noticing improvement within the first few treatments. The following is a short incomplete list of problems that might be discovered in the exam. Rotator cuff dysfunction including strain, tendonitis (inflammation), tendinosis (adhesions), impingement (pain when lifting arm away from or behind body), bursitis (inflamed bursa sacs that are irritated from friction), and adhesive capsulitis (frozen shoulder). Other musculoskeletal problems of the shoulder might require more advanced diagnostic testing such as x-rays, MRI’s and CT scans and may capture tears, arthritis (several kinds), avascular necrosis, fractures, infections, and tumors. Rotator cuff muscles of the shoulder (they are the core muscles in the shoulder and responsible for stabilizing and moving the joint is several planes of motion). There are non musculoskeletal problems that may contribute to shoulder pain as well and should be ruled out prior to treatment. Conditions such as gallbladder disease which classically refers to the right scapulothoracic region and of course heart attacks have been known to refer pain to the left shoulder as well the mid back region. Lung conditions such as a blood clot (pulmonary embolism), infection, and tumors may also refer to the shoulder region. Other internal organs may refer pain to the shoulder including pancreatitis, an ovarian cyst, and an ectopic pregnancy to name a few. Thankfully, non musculoskeletal shoulder pain is the exception and not the rule. In my office, I collaborate with other specialists if we are suspicious of chronic shoulder pain that does not respond to conservative care and may be from non-musculoskeletal sources. Fortunately, most shoulder problems are mechanical in nature and are the result of either muscle tightness, adhesions, and joint restrictions in the neck and upper back. Repetitive stress from poor posture and ergonomics will contribute to shoulder pain slowly and insidiously over time. This is why many patients will say that it just came “out of nowhere” usually upon awakening from a night's sleep. It is not the fact that they “slept wrong” but rather the poor mechanics they use while they sit, stand, and sleep over a period of time. This will ultimately cause an imbalance in the neck, upper back and shoulder region. It is often accompanied by a shoulder impingement. Shoulder impingement is a reduction in the gap between the ball and socket where one of the rotator cuff muscles slides through. The rotator cuff muscle becomes impinged especially when raising the arm horizontally or attempting to put a coat sleeve on. The good news is that after a detailed exam that includes range of motion of the neck, upper back, and shoulder followed by testing of all the muscles that cross the shoulder and palpating (clinically feeling) each structure a working diagnosis can be made and a treatment plan can be mapped out. If the “shoulder” problem is mechanical, and most of them are, a treatment plan that includes joint and muscle manipulation followed by therapeutic exercise at home, and health counseling can be made. The treatment plan will be a relationship between the practitioner and the patient and will consist of therapies in office and exercise prescription at home. Progress is the key! Great results can be expected within 4-6 weeks. Usually, treatments are 1-2 times a week and home therapies prescribed daily. Below are some pictures and treatments of the shoulder. This is a sample of some care and does not represent a treatment plan for the shoulder Specific high velocity shoulder manipulation to the glenohumeral (shoulder) joint (this requires a high level of expertise and is only performed on certain conditions that warrant it- i.e. subluxation or impingement syndrome of shoulder) Soft tissue manipulation to one of rotator cuff muscles (subscapularis) under the shoulder joint Myofascial release using a lacrosse ball (this can be part of self care at home- find the sore trigger points and gently apply pressure with the body over them for 5-10 seconds. Should feel slightly uncomfortable but a good pain. Pain scale when doing it should be a 3 or 4 out of 10. If it is a 5 out of 10 that is too much pressure. Therapeutic exercises for shoulder pain: Assisted shoulder stretches(this is a general range of motion exercise) Rotator cuff theraband exercises (internal rotation) Working both shoulders simultaneously develops symmetry
Dr. William Brightman DC, MS, MEd Chiropractor & Exercise Physiologist Private Practice in Mahopac By William Brightman
It is not uncommon for individuals with low back pain to avoid all activities. On the surface this might seem intuitive, however; in reality, it is not such a good idea. The prevailing thought for nearly 100 years was that when you have back pain you need to rest. That might be true if the pain is moderate to severe (on a pain scale of 1-10 your pain is greater than a 6), but even with intense pain it is important to get some form of “pain free” activity. One of the most common themes of activity avoidance is that the individual will do nothing for days or even weeks. At that time, they may feel better and as soon as they go back to their “normal” activities then the pain returns. So what do they do - they rest again or take medications to try and block the pain and “work through it”. This is not the answer. Most of the literature today supports a gradual return to normal activities with low back pain. The focus is to do activities that help heal the pain while preventing the inevitable deconditioned syndrome. When muscles are not used they begin to atrophy and become weaker. This cycle will perpetuate itself even when the individual returns to their normal activity. The key to returning to your normal activities is to get the care you need for starters. Consult a practitioner who understands the condition and can help guide you back to your normal activities with treatment and modified activities to help strengthen and support while reducing the low back pain. One of the most effective treatments for acute low back pain is spinal manipulation. The literature is overwhelming in support of this approach to managing low back pain. Usually within the first few treatments the patient is experiencing relief. Once you are feeling around 50% better, then this is where therapeutic exercise is critical. Therapeutic exercise is a combination of flexibility, strengthening, and balance. These pain free activities are encouraged to be done daily and should be of low intensity for relief care. Once the patient is feeling significantly better then there can be a resumption of normal activities. It is highly recommended that physical activities include aerobic exercises as this form of exercise helps to mitigate low back symptoms in the long haul. There are studies that show that once the acute pain is better, activities that are aerobic in nature may be effective at managing chronic low back pain. In fact, in a large scale study of 4,246 Finnish men and women (average age 34), those who engaged in multiple activities and sporting events- especially aerobic (cycling, walking, hiking, running), had reduced radiating and non radiating back pain when compared to those who just focused in on one exercise. The conclusion is that a variety of exercises and activities are probably best as opposed to just one ‘target’ exercise such as low back stretching. Another study analyzed 4,022 middle aged men who demonstrated a clear relationship between chronic low back pain and low physical activity level. The findings persisted even after researchers controlled for obesity which is another risk factor in chronic low back pain. Another study done this year analyzed 7,565 older men and the results were similar. In this study the researchers calculated total movement during the day and chronic low back pain. You guessed it. There was an inverse relationship between movement and chronic low back pain. The more they moved (within reason) the less low back pain they had. My advice is get the care you need, feel better, do the basic stretches and strengthen the low back. Once you are 50% better, begin to add different modes of aerobic and physical activity. Walking, hiking, elliptical, rowing, cycling, weight training, theraband work and even gardening will help manage your chronic low back issues. Do these activities 4-5 times a week for 30 minutes and check in with your sports chiropractor and you will have managed your back pain conservatively, while conditioning your body. William Brightman DC, MS, MEd Sports Chiropractor and Exercise Physiologist Private practice in Mahopac, NY Educator of Sports Medicine and Professor of Anatomy & Physiology William Brightman DC, MS, MEd The statistics are pretty staggering. About 80% of all adults will suffer from low back pain. It is one of the leading causes of disability globally. It not only prevents people from doing their job but also limits other activities of daily living. This single handedly impacts overall health and can lead to long term disabilities. Back pain accounts for more than 264 million lost work days in one year and it does not discriminate against age or gender. It strikes kids, adults, and the elderly. Low back pain is not only crippling to the one suffering but also can be damaging to the economy with upwards of 100 billion in lost wages and decreased productivity. Moreover, it will play an emotional toll on the sufferer and their family. As overwhelming as the statistics are these numbers can be greatly reduced with conservative care, collaboration with other specialists, and lifestyle modifications. There are so many types of low back pain, hundreds of causes, and many approaches to managing the different types of pain. From medications to injections, physical therapy, chiropractic care, weight loss, acupuncture, counseling, nutrition and of course, surgery, it is no wonder why a patient might be confused as to what path to take. As a sports chiropractor I generally get a large variety of musculoskeletal complaints in my office. I have patients who present with injuries from the bottom of the kinetic chain (foot/ankle) to the top of the chain (neck). The injuries may be sport related,from repetitive stress, or from inactivity. Even though I manage different conditions throughout the body, I am still bombarded with the number one complaint by patients- low back pain. It is always important to do a complete physical exam to rule out any underlying condition. Most low back pain is mechanical in nature- meaning that it arises from muscles, tendons, ligaments, disc, or nerve. Some of it is local to the low back only and others are radiating to the lower extremity. With radicular symptoms I will often order an MRI or consult with a spine specialist who might perform an EMG/ NCV (electromyography nerve conduction velocity) test. While I typically manage most of my patients who suffer from low back pain in the office, I will collaborate with other medical specialists when I feel that the patient needs a multi disciplined approach. Mechanical back pain is usually the result of a sprain/ strain with some kind of joint dysfunction (i.e. facet syndrome), but it may also be related to a disc displacement. The latter is more severe and takes considerably longer to heal with the right treatments in place. The causes of low back pain can be obvious like an athletic injury, motor vehicle accident or lifting a very heavy object. But it can also occur from just moving the wrong way. Poor posture, desk workers, obesity, and arthritis are other factors that can set you up for low back pain. Sometimes low back pain can arise from internal structures such as ovaries, kidneys, and prostate problems as well as focalized cancers, bone disease, and infections to the area. This is why diagnosis is always first and foremost. Thankfully, these internal problems are not common. Most mechanical causes of low back pain can be managed nicely with chiropractic care including spinal manipulation, muscle work, and corrective exercise. There is a growing emphasis on quality care, clinical outcomes and cost effectiveness as well as non drug approaches to managing low back pain. Chiropractic care fits nicely into this need, especially in light of the abuses from prescription opioid use. There is overwhelming evidence reported from the following prestigious journals recommending chiropractic care as a first defense in the treatment of low back pain. Agency for Health Care Research and Quality; Annals of Internal Medicine; Medical Journal Spine; and Journal of American Medical Association to name just a few. This is in addition to countless other journals and thousands of clinical studies that have all recommended chiropractic care in the treatment of acute and chronic low back pain. Most patients with mechanical back pain start feeling better within the first few visits. This combined with therapeutic exercises and lifestyle modifications the patient will continue to function better during their normal activities with less pain. Chiropractic care may have to be utilized with high frequency the first few weeks for long term sufferers, but after that initial phase, only maintenance may be needed to manage chronic low back pain. This beats the alternative of chronic pain and/or drug use! Some cases of acute low back pain resolve within 1-5 treatments and do not need additional chiropractic care. The spinal manipulation improves joint mobility and range of motion while reducing pain. This combined with a home stretching and strengthening program of 10 minutes 3-5 days a week will enhance the results. Stretching and Physical therapy alone can be beneficial to certain types of low back pain- but when combined with specific chiropractic manipulation the results are superior. Pain relief within 24-48 hours with improved mobility is the outcome. The following is a list of other recommendations in addition to chiropractic manipulation and home exercise for the treatment and management of low back pain. They are as follows:
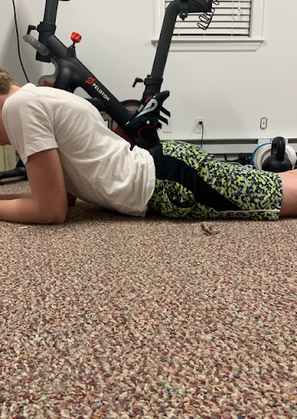
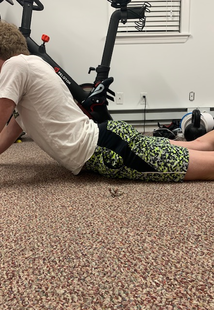
Spinal manipulation that incorporates flexion distraction or decompression (left) combined with high velocity adjustments are very effective in managing acute and chronic low back pain. An overcorrection with posture to increase awareness to all postural muscles. (A plumb line can be drawn through the ear, shoulder, hip and ankle) Correct seated posture is important in preventing back and neck pain. Slumped position on the left increases strain on spine while correct posture with lumbar support decreases load throughout the spine (low back and neck) Below are some helpful stretches and strengthening exercises for the low back. Foam rolling to loosen soft tissue “tightness” (L): hip extension to activate gluteus maximus which is beneficial to low back (R) Lumbar spine extension exercises off a physioball combined with bridges are excellent at strengthening the deep core spinal muscles. Knee to chest with a cross over stretch to help lengthen lumbar muscles: Exercises like this can be done very early in care for relief. Spinal extension and flexion exercises (Cow-cat exercises) Opening up the hips helps to unload the low back Variations of spinal extension stretches and strengthening exercise
There are an assortment of different strengthening and stretching exercises that when combined with hands on manipulation, physical therapy, and different modes or aerobic exercise can be very effective at managing both acute and chronic low back problems. William Brightman DC, MS, MEd Private Practice, Mahopac NY [email protected] William Brightman DC, MS, MEd Neck pain is one of those conditions that can come out of nowhere or is the result of a trauma such as “whiplash” from a motor vehicle accident or an athletic injury. Oftentimes, neck pain comes on insidiously and the sufferer usually will attribute it to “how they slept”. While sleeping the wrong way can certainly contribute to a pain in the neck it is often not the cause. Poor posture and repetitive stress are the most common causes of neck pain. Moreover, neck pain can also stem from other parts of the body such as the low back or even the upper back. Neck pain that comes out of “nowhere” usually stems from that poor posture we all fall prey to when we are seated at our desktop and our head is jutted forward placing an increased strain on the neck. It may start out as generalized stiffness or soreness and progress to pain and loss of motion. This type of pain will mostly impact the muscles and the joints in the cervical (neck) region. However, disc and nerve problems can also occur with prolonged neck pain. With disc pain the patient may also feel pain, numbness, and/or a tingling sensation radiating down the arm. Poor posture will often occur when we are texting or using a tablet and are not focused on the position of our neck. There is a condition called “text neck” that explains how when we are texting our head is usually flexed downward which puts increased strain on the muscles in the posterior region of the neck. Tablet users who are younger and who do not have a dedicated workspace will find themselves in positions of compromise for hours. Holding one position for extended periods of time is not only bad for the neck but will impact the entire spine. In fact, lying in a face down or prone position up on elbows will strain muscles and joints in the low back and neck. A slouched position on the couch will inevitably work its way from low back to the upper back and neck. When all the curves of the spine are impacted then any one of them can result in pain. The best approach to treating neck pain is to have a health care professional who specializes in spinal care perform a complete exam of the cervical spine and all associated structures. An exam that includes neurological and orthopedic assessments along with general palpation (clinically feeling) of different muscles and joints will help determine what structures are impacted. Once the exam is complete it is sometimes necessary to order x-rays to rule out any bony and joint abnormalities. X-rays are not that clinically useful unless there is a suspicion of a bone issue. Misalignments can be diagnosed with a physical exam and plain films are not necessary. If there is radiating arm pain with numbness an MRI may be ordered to rule out a disc injury. This is only necessary if it is clinically prudent and the treatment is not working and further diagnostics are necessary. I am a firm believer in not ordering unnecessary testing out of “fear of missing something”. Once the diagnosis is made a treatment is mapped out to help alleviate the neck pain. With sprain/strain and joint problems I find gentle chiropractic adjustments and muscle work (massage and myofascial release) are very effective at managing the pain. Usually within the first week the patient is feeling much better (1-3 treatments). Physical therapy modalities that combine ice/heat and other modalities may also be helpful. Guided home exercise that includes stretching and strengthening of the neck and upper back muscles is provided to the patient. Advice with postural positioning such as sitting in a chair with lumbar support and having a tablet just below eye level is recommended. It is best to keep your head upright and have arms relatively close to the body as to not stress shoulder/upper trapezius muscles. It is important not to fall back into the same trap of poor posture from sitting, sleeping, or text neck! Below are some helpful exercises to help in the management of neck pain secondary to repetitive stress. Gentle stretches followed by slow theraband strengthening exercises for the neck
William Brightman DC, MS, MEd Chiropractor Private Practice Mahopac NY [email protected] By William Brightman DC, MS, MEd
We certainly know that a good night's sleep certainly can help boost your energy, spirits, and overall well being the next day. Waking up refreshed and ready to go is truly a gift. Unfortunately, there are millions of people waking up each day unrefreshed, in pain, with little energy to move forward throughout the day. The National Institutes of Health estimates that approximately 30 percent of the general population complains of sleep disruption, and approximately 10 percent have associated symptoms of daytime functional impairment consistent with the diagnosis of insomnia. Insomnia is a crisis and there are many reasons for it. Needless to say stress is probably at or near the top of the insomnia equation. Other causes of insomnia include medical conditions, depression, and lifestyle to name a few. Insomnia is extremely complex and those who are suffering should seek council from an expert in the field. Insomnia tends not to go away on its own and it is critical to get to the underlying problem. The intent of this article is to highlight one medical condition that may be contributing to sleep disruption which can lead to insomnia and other ill effects on the body. Musculoskeletal pain has a reciprocal impact on sleep. In other words, individuals who have a sleep disorder are more prone to musculoskeletal pain and people who have musculoskeletal pain are more likely to suffer from insomnia. This may be difficulty falling asleep because of pain, waking up during the night secondary to pain, or not being able to fall back to sleep due to the pain. It can play out in several different scenarios. The bottom line is the pain is not getting better, the individual is more likely to develop other health problems in response to the sleep disruptions, and the problem becomes cyclical and more entrenched the longer you avoid treatment. Chiropractic care has been studied in populations that have sleep disturbances. One population is people who suffer from fibromyalgia. Studies demonstrated that consistent chiropractic care helped these patients with not only pain but better quality sleep. Other studies have shown that patients whose sleep disturbance is related to their spine have benefited greatly from chiropractic care. If musculoskeletal pain is the root cause of the sleep problem then natural care such as chiropractic can offer mitigation of symptoms and allow the individual to sleep more soundly. Furthermore, your chiropractor can offer a lifestyle council with diet and exercise to help the patient who suffers from sleep disruption. Obesity is directly correlated to sleep apnea and these patients need council on weight management. I will refer out to a nutritionist for dietary assistance, and refer out to an experienced personal trainer who has helped clients with weight management in a safe manner that does not stress their joints too much. Individuals who eat late at night, drink alcohol, smoke, and have caffeine are more likely to suffer from insomnia. There are also medications that disrupt the circadian rhythm. Sometimes there are simple solutions to the problem. Unfortunately, food and alcohol are tied into addiction and the problem may be deeper than just a lifestyle modification. A visit to the mental health counselor may be in need for therapy and program changes! There are a lot of natural remedies such as melatonin (hormone made by the pineal gland that helps support circadian cycles- sleep- wake cycles), theanine (an amino acid that helps reduce anxiety), magnesium (deficiencies have been associated with sleep disorders, anxiety, and heart irregularities), valerian root (increases neurotransmitter GABA that helps with calmness). Each of these may benefit the sleep sufferer. A good mattress that is firm and pillows to keep your body in natural alignment are also very helpful in a good night's sleep! The bottom line is sleep and associated sleep disorders are very complex. As a chiropractor I would only make suggestions and offer treatments that I think may help my patient sleep more soundly. If the root of the problem is musculoskeletal pain and I can help with manual therapies and other modalities then it is a win win! When the patient feels less pain and sleeps better, that is music to my ears!. However, it is recommended that patients seek a specialist to help with more serious sleep disturbances. In the meantime, a chiropractor, some lifestyle council (diet and exercise), and maybe a supplement like melatonin and magnesium may do the trick! William Brightman DC, MS, MEd Sports Chiropractor & Exercise Physiologist Private practice Mahopac NY [email protected] |
AuthorDr. William Brightman has been a practicing chiropractic physician since 1998 and has been in health promotions since 1989. He currently has a successful private practice in Mahopac, NY, where he specializes in the diagnosis and treatment of joint and muscle pain. ArchivesCategories
All
|


















































































 RSS Feed
RSS Feed
